Predictive analytics doesn’t just offer a path to increased short-term revenue. Ultimately, it empowers providers at your organization to offer stronger care — which is the only way to grow sustainably in the healthcare industry.

A 2023 report from FinThrive found that RCM leaders are adopting analytics technology at an extremely high rate: between 80% and 90% in the areas of A/R analytics, claims analytics, collections analytics, and coding analytics. In a recent survey conducted by Black Book Research, 76% of healthcare CFOs planned to dedicate 10% or more of their technology budgets to predictive RCM analytics, and that number is likely to continue to rise. Only 7% of CFOs had no plan to implement predictive analytics.
The takeaway is clear: To stay ahead of the curve, your organization must harness the power of predictive analytics.
Our mission at Revco is to propel health systems and hospitals toward unprecedented financial health through RCM success. To that end, we’ve compiled all of the essentials around predictive analytics: what it is, the key metrics that it involves, and most importantly, how you can leverage it to enhance your RCM performance.
What Is Predictive Analytics?
Predictive analytics helps you anticipate and prepare for future trends and patterns.
Predictive analytics can be thought of as an insight-extracting machine: massive quantities of data go in, an array of algorithms sift through the data, and high-accuracy projections come out. In the realm of RCM, this might look like:
- Segmenting patients by their propensity to pay,
- Forecasting cash yields from accounts receivable (A/R), or
- Anticipating how payers might change their rules for the adjudication of claims.
As you’ve likely learned during your years of RCM experience, each of these predictions implies a tangible next step. Once you understand a patient’s ability to pay, you can maximize efficiency by focusing collection efforts on high-return patients instead of those who may be eligible for charity. With a better grasp on short-term cash flow, you’re able to invest in the right strategies for patient care. If you know how a payer will alter their rules, you can make proactive changes to minimize denials under their new guidelines.
How you make those decisions falls under the purview of prescriptive analytics (which we’ll touch on later), but for now, it’s crucial to understand that these “next steps” will remain invisible until you enlist predictive analytics to reveal them.
How RCM Leaders Leverage Predictive Analytics
Naturally, RCM leaders are seeking to use predictive analytics to enhance collections, avoid denials, and optimize the various facets of their RCM strategy. But there are deeper reasons behind the push for analytics.
According to Black Book Research, the driving reasons behind acquiring RCM analytics tools in the near future include:
- Predicting payer remittance dates to manage organizational cash flow,
- Flagging potential denials before they occur,
- Identifying inefficiencies and breakdowns in RCM processing at early stages,
- Using machine learning to predict changes in payer-specific rules for claims adjudication,
- Reducing dependency on IT resources for accessing the information you need,
- Streamlining the RCM each fiscal year, including acquisitions and contract changes,
- Identifying organizational-specific indicators for RCM leakages and strengths, and
- Supporting patient engagement goals by refining processes impacting patient payment.
While each of these outcomes is desirable, they won’t come about without precise, persistent effort from your RCM team. To ensure that you’re getting the most out of your analytics initiative, you need to know which specific metrics to track — and how to refine them for targeted success.
performance-driving RCM insights?
Key RCM Metrics Enhanced by Predictive Analytics
Let’s unpack a few of the metrics that are integral to predictive analytics. (Keep in mind that these metrics are representative, not exhaustive! For a comprehensive walkthrough, check out our breakdown of the most important KPIs for revenue cycle performance.)
Denials Management KPIs
Crucial KPIs that will help you minimize claim denials include:
- Anticipated claim denial rate: The percentage of submitted claims that payers are likely to deny based on past data. Though the industry average is between 5% and 10%, you should aim to keep your claim denial rate as low as possible.
- Anticipated clean claims rate: The percentage of submitted claims that are likely to be paid without any edits. Because modifying claims saps energy from your organization, you should strive for a clean claims rate that exceeds the industry benchmark of 98%.
- Projected net collection rate (NCR): The percentage of payment you receive compared to what insurance companies contractually owe you. Your organization should seek an NCR of 95% or higher.
Debt Collection KPIs
- Propensity to pay: How likely a patient is to pay their debt. At Revco, our proprietary propensity-to-pay model considers volumes of data (for example, payment history) then assigns a score to each patient to help us prioritize high-ROI accounts for collection.
- Anticipated right party contact (RPC) rate: How often collection calls reach the intended recipient. Getting this number close to 100% is a simple yet effective way to improve collection efficiency.
- Projected average payment per call: How much money your RCM department recovers on a call-by-call basis. If you can accurately project this metric, you can plan outreach methods accordingly and make informed budgeting decisions.
Organizational KPIs
- Future cash flow forecasts: How much cash your organization is likely to recover within a time-bound target (month-end, quarterly, etc.). Mastering this metric will help your organization make prudent investments — not just in the RCM arm, but throughout the whole process of care delivery.
- Strategic predictions: A wide range of metrics that will help your RCM team sharpen its strategy. For example: Which training initiatives have been most successful for collectors? If your collectors have perfected the art of compassionate outreach, you’ll maximize your revenue while maintaining the trust you’ve built with your patients.
Benefits of Predictive Analytics in RCM
With careful planning, precise execution, and constant refinement, predictive analytics will bring a wealth of short- and long-term benefits to your organization.
Proactive Decision-Making
In the words of English priest Thomas Adams, “Prevention is so much better than healing because it saves the labor of being sick.” This adage rings true in RCM. Of course, solving problems drains precious resources from your organization — but the real loss is the revenue that dissipates before you even identify the problem.
Predictive analytics is the solution. It sheds light on potential problems before they arise, allowing you to swiftly enact training, protocols, and revamped processes to avoid those problems (and the loss of revenue that they entail).
Deeply Informed Strategy
One of the luxuries of living in the “data economy,” as IBM puts it, is that you no longer have to guess which strategies will work. You can trust machine learning and AI to uncover insights from vast swaths of patient data, and you can calibrate your strategy based on what your tools reveal.
Remember: Guesswork has no place in a data economy. And it certainly has no place in the information-rich realm of RCM.
Enhanced Patient Experience
Though the immediate benefit of predictive analytics in healthcare is a boost in revenue, the ultimate benefit of analytics is far more crucial: Analytics empowers your ability to deliver care.
Predictive analytics strengthens patient outcomes in two ways:
- Analytics enhances the patient experience. In your collection efforts, it can help you understand the outreach method (call, text, chat, etc.), tone of voice (encouraging, educating, understanding, etc.), and collection strategy (pay in full, payment plan, redirection to financial counseling, etc.) that will help patients form a favorable view of your brand.
- An analytics-fueled increase in revenue equips your organization to hire the best healthcare providers and purchase cutting-edge equipment, which elevates the most important elements of care: physical and mental well-being.
A Foundation for Sustainable Growth
A robust predictive analytics platform will help you collect additional revenue from patients and payers. But the key to lasting success in your RCM department and throughout your organization is creating happier, healthier patients. As we saw above, investing in analytics unlocks funds that can be invested in stellar patient care, powering your revenue cycle toward tremendous success.
Predictive Analytics: Integral to a Data-Driven RCM Approach
Though our focus has been on the predictive variety of analytics, there are four primary types of analytics in RCM. Each is equally crucial for improving performance, and your organization cannot reach its full potential without achieving harmony between the four types: descriptive, diagnostic, predictive, and prescriptive.
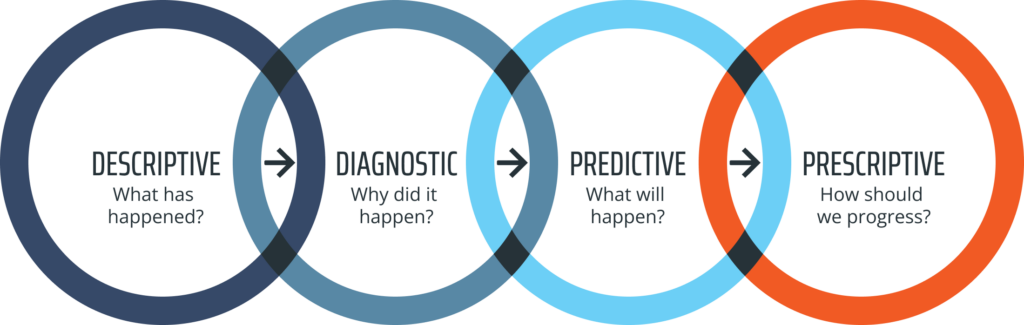
Let’s do a quick walkthrough of each.
–––––––
Descriptive Analytics
Descriptive analytics uncovers trends from past data. It illuminates areas where work needs to be done, answering questions like:
- Why are our claims getting rejected?
- Which payers are most likely to reject our claims?
- Which outreach methods have been most successful with younger patients?
- Which of our collector training programs has been most effective?
Diagnostic Analytics
Diagnostic analytics dives deep into the root cause of RCM problems. It ensures that you don’t stop with a surface-level explanation by addressing questions like:
- Which diagnoses are most likely to require additional information to resolve a claim?
- What practical impact have recent changes to the adjudication process had on our denials management results?
- Why is a phone call the best outreach method for older patients — and how does this affect our cost to collect?
Predictive Analytics
Predictive analytics projects future patterns and trends in RCM. With a strong foundation of past insights from descriptive and diagnostic analytics, your organization can move to questions like:
- Which payers are most likely to respond favorably to appeals?
- How much aged debt are we likely to recover by the end of the month?
- How will wide-scale trends in patient health — for example, the COVID pandemic — impact the types of claims we submit and the likelihood of patients paying their bills in full?
Prescriptive Analytics
Prescriptive analytics recommends the best strategy going forward. Now that you’ve extracted insights from the past and peered into the future, you’re ready to answer the million-dollar question:
- How do we turn what we’ve learned into improvements that meaningfully impact our bottom line?
Depending on what you’ve uncovered during the descriptive, diagnostic, and prescriptive phases of investigation, this might look like:
- Training collectors to gently educate patients on their bills,
- Improving your documentation procedures for one particularly picky payer,
- Creating a podcast that connects with other high-level healthcare leaders, or
- Partnering with an RCM agency that will generate maximum revenue by harnessing the power of analytics.
Transform Data Into New Revenue with Revco
At Revco, we’re driven by outperformance. We believe that analytics isn’t just the future of RCM success — it’s the key to outpacing your competitors and delivering superb patient care today.
We’d love to partner with your organization through our analytics-driven early out, debt collection, and denials management services. If you’re ready to pursue unprecedented financial health, start a conversation with us today.






