
AI is transforming the patient billing experience by reducing errors, increasing transparency, and giving patients more confidence in their financial journey. For healthcare systems, adopting AI doesn’t just reduce administrative burden—it strengthens patient trust, accelerates payment turnaround, and enhances long-term loyalty.
Contact Revco to see how our utilization of AI can help your healthcare organization!
Table of Contents
Introduction: Patient Billing is the Most Lasting Impression of the Care Experience
For many patients, the billing experience is the final chapter of their healthcare journey. It comes after the diagnosis, the procedure, and even the follow-up care. For providers and health systems, billing is not just a transactional step—it’s a trust-defining moment.
When billing feels confusing, inaccurate, or adversarial, patients remember. The result? Lower satisfaction, delayed payments, and an increased risk of patients deferring future care.
In fact, a recent survey showed nearly half of insured, working-age adults have received a bill or copayment in the past year for a service they believed was already covered by insurance. Less than half of the respondents challenged their bill, and those who did found a significant delay in receiving care, ultimately causing their health condition to worsen while they awaited resolution.
With the rise of artificial intelligence (AI), healthcare organizations now have the opportunity to redesign this critical touchpoint. By using AI to bring clarity, automation, and self-service tools to billing, providers can reduce patient anxiety and reinforce their reputation as trusted partners in care.
How Billing Anxiety Impacts Patient Retention
A patient’s financial experience has as much impact on loyalty as their clinical care. In a 2021 healthcare consumer survey, 93% of respondents said the quality of their billing and payment experience influences whether they will return to a provider. In a separate 2023 survey, 56% of patients said they would consider switching providers after a poor billing experience. These findings underscore how financial transparency and clarity are now core drivers of patient loyalty.
Billing anxiety can manifest in:
- Delayed or avoided payments due to confusion.
- Higher inbound call volumes as patients try to clarify balances.
- Lower trust in the provider when surprise bills occur.
- Deferred care when patients worry about affordability.
AI can directly address these pain points by making billing more predictable, transparent, and error-free.
AI doesn’t just reduce billing errors—it reshapes the patient financial experience. Health systems that adopt AI-driven billing build stronger trust, accelerate cash flow, and create a competitive advantage in patient loyalty.
Conversational AI: Self-Service That Patients Expect
Patients are increasingly expecting the same level of seamless, personalized, and proactive support they receive from other consumer tech —like Apple or Amazon.
A recent study found that 70% of patients want to pay their healthcare bills online, but nearly half of healthcare providers still process claims manually. As a result, bills are delayed, ignored or disputed, and the collections process becomes more painful for everyone involved. The lasting impact is patient dissatisfaction. By incorporating AI through chatbots, text, or voice-enabled tools, providers can provide patients with more options like:
- Check balances in real time.
- Set up payment plans.
- Get quick answers about insurance coverage.
- Receive reminders and confirmations automatically.
For health systems, this reduces call center volume, lowers staffing strain, and speeds up payment resolution. For patients, it creates an experience that feels supportive, not stressful.
AI for Billing Accuracy, Transparency, and a Faster Revenue Cycle
Accuracy in billing is non-negotiable but manual processes, missing data, and outdated systems often create costly friction. For patients, that means confusion, surprise bills, and frustration. For providers, it means rework, denials, and delayed revenue. AI addresses these challenges by creating a clearer, more reliable financial experience for everyone involved.
Benefits at a glance:
- Reduced errors & denials
- Faster payment turnaround
- Improved patient trust & loyalty
- Streamlined registration & claims processing
How AI strengthens billing and the revenue cycle:
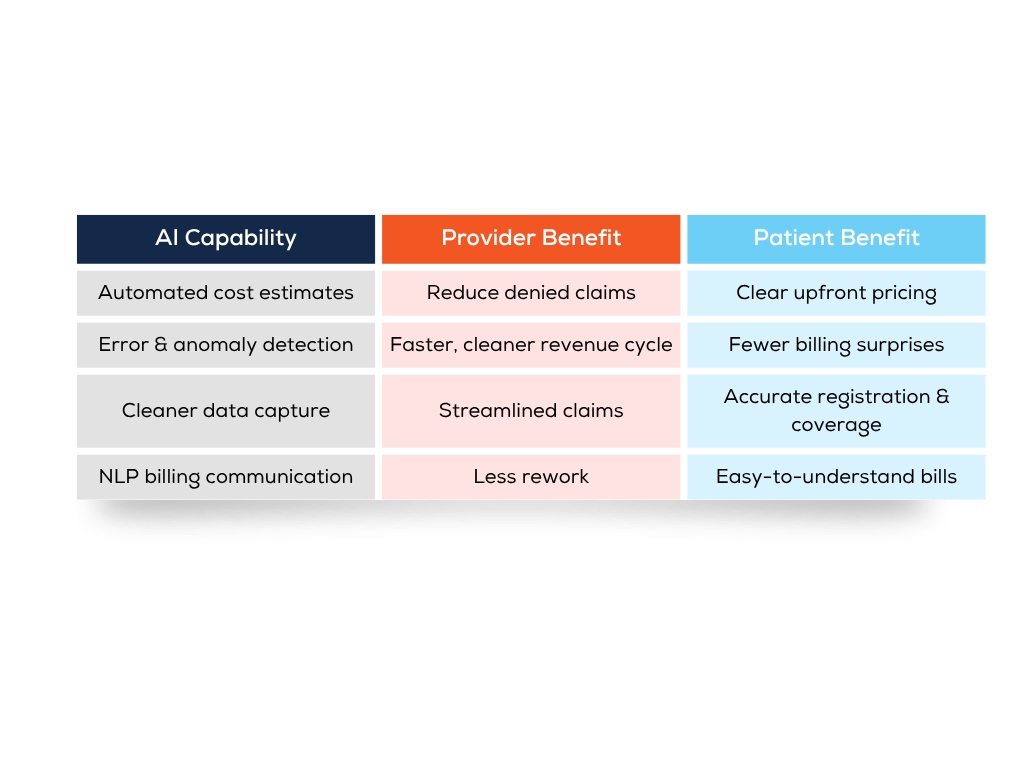
- Automated cost estimates: By pulling from payer contracts, patient coverage details, and historical data, AI delivers more accurate upfront estimates. Patients are better prepared financially, and providers reduce the likelihood of surprise bills.
- Error and anomaly detection: Machine learning models flag mismatches or unusual patterns before claims are submitted, cutting down on denials, rework, and compliance risks.
- Cleaner data capture: AI verifies demographics and coverage during registration, reduces duplicate or incomplete records, and streamlines prior authorization tracking, ensuring claims are accurate the first time.
- Patient-friendly communication: Using natural language processing (NLP), AI can translate technical claim language into clear, accessible explanations, helping patients understand their bills without the stress.
The result is a billing process that patients understand and trust—leading to fewer complaints, faster payment turnaround, and stronger provider reputation. At the same time, health systems benefit from cleaner claims, shorter cycles, and more efficient revenue recovery.
How Revco Supports Patient-Centered Collections
At Revco, we understand that billing isn’t just about dollars. Our approach combines advanced analytics and patient-focused communication to reduce financial stress while ensuring providers recover revenue efficiently.
From insurance revenue recovery to patient-friendly collections, Revco helps health systems strengthen patient trust while improving bottom-line results.
Q&A: What Healthcare Leaders Need to Know About AI in Billing
Will AI replace human billing teams?
No. AI is designed to enhance, not replace, revenue cycle staff. It automates repetitive tasks and reduces errors, allowing teams to focus on complex cases and patient engagement.
How does AI impact patient trust?
By providing clear estimates, accurate bills, and easy-to-use self-service tools, AI builds confidence that the provider is fair and transparent. AI-powered self-service tools also make the payment process easier and more accessible, improving the overall patient experience.
What’s the ROI of AI in billing?
Health systems see value in multiple areas: fewer denials, faster payment turnaround, lower staffing costs, and improved patient loyalty, all of which contribute to faster cash recovery and more sustainable financial performance.
Is conversational AI secure for patient data?
Yes. Leading AI platforms are HIPAA-compliant and use encryption to protect patient information. Security and privacy remain foundational.
How quickly can health systems adopt AI in billing?
Many tools integrate with existing EHR and RCM platforms, allowing for phased implementation. Providers can start with simple automation (like estimates or reminders) and expand into more advanced workflows.
How can AI improve healthcare billing accuracy?
AI reduces human error by verifying patient demographics, insurance coverage, and historical claims data. Machine learning models flag anomalies before submission, minimizing denials and rework. Providers using AI for medical billing accuracy report faster payment cycles and fewer billing disputes.
Can AI help patients understand their medical bills?
Yes. AI-powered tools and natural language processing (NLP) can translate complex claim language into patient-friendly explanations. This increases transparency and trust, reduces billing anxiety, and encourages timely payment.
How is AI used in revenue cycle management (RCM)?
AI supports RCM by automating cost estimates, identifying potential denials, and cleaning claim data. This improves first-pass claim accuracy, shortens the revenue cycle, and ensures providers recover more revenue efficiently.
How can conversational AI or chatbot solutions support patient billing?
Conversational AI enables self-service billing support. Patients can check balances, set up payment plans, and get answers to insurance questions in real time. This reduces call center volume and improves the patient financial experience.
How does AI help prevent surprise medical bills?
By using real-time payer contract data, AI can provide accurate cost estimates upfront. Patients see what they owe before care, which reduces confusion, surprise bills, and deferred visits.
Why should healthcare executives consider AI for billing?
AI tools align financial performance with patient-centered care. CFOs and revenue cycle leaders benefit from AI through improved operational efficiency, reduced errors, enhanced patient satisfaction, and stronger retention. These tools can also alleviate administrative burden, reducing staff burnout.
Conclusion: Trust, Satisfaction, and Sustainable Growth
The billing process is no longer just an operational function; it’s a reputational one. Patients are judging their overall healthcare experience based on whether their financial interactions feel transparent, accurate, and supportive.
AI gives health systems a clear path forward: fewer errors, cleaner data, faster resolution, and most importantly, higher patient satisfaction.
For C-suite leaders, investing in AI-driven billing isn’t optional—it’s essential for retaining patients, safeguarding reputation, and ensuring long-term sustainability in a competitive healthcare market.
Contact us today to see how we can help you recover more—faster and smarter.






