Chatbots, data analytics, coding and billing programs—artificial intelligence (AI) is already present in many aspects of the healthcare revenue cycle.
But like any new technology, AI tools must be properly vetted and staff must be trained to use them before they can offer real value. The essential question should always be: Is this tool enhancing the patient experience?
Let’s take a closer look at some of the best ways to use AI and machine learning in revenue cycle management, along with the potential pitfalls your leadership team needs to know.
Applications of AI in Healthcare Debt Collection
Given the amount of administrative work that healthcare RCM necessarily involves, AI does have a variety of highly useful applications in this space.
As with any new tool or process, however, you’ll want to keep a close eye on how it’s working for your team. If it proves disruptive to your patients, or if it negatively impacts the level of service you can provide, it’s important to be open to changing course. As we’ll see throughout this piece, AI initiatives must be balanced with a deft human touch to ensure that your patients’ financial experience is characterized by compassion and excellent care.
With that said, let’s explore which types of RCM tasks are a good fit for AI.
Patient Billing and Payments
Billing and payments are one of the most popular areas of use for artificial intelligence.
In fact, you’re probably already using some form of AI here. For example, if your organization sends out automated text or email reminders for patients on payment plans, that’s powered by AI. If you have a chatbot available to answer simple billing or payment questions, that’s also AI.
But artificial intelligence can be used for more complex, high-value tasks as well, like creating personalized payment plans.
Research has shown that consumers like payment plans: a 2021 PYMNTS report found that 63 percent of patients expressed interest in the option, and 33 percent said a payment plan would entice them to switch medical providers. An AI tool can easily create a flexible patient payment plan by drawing on patient financial data and quickly creating different options based on timeline or payment amount. With these AI-guided payment plans in hand, your staff is equipped to walk patients through what each plan entails, and help them pick the option that’s the best fit for their specific financial circumstances.
Reduce Manual Errors and Administrative Work
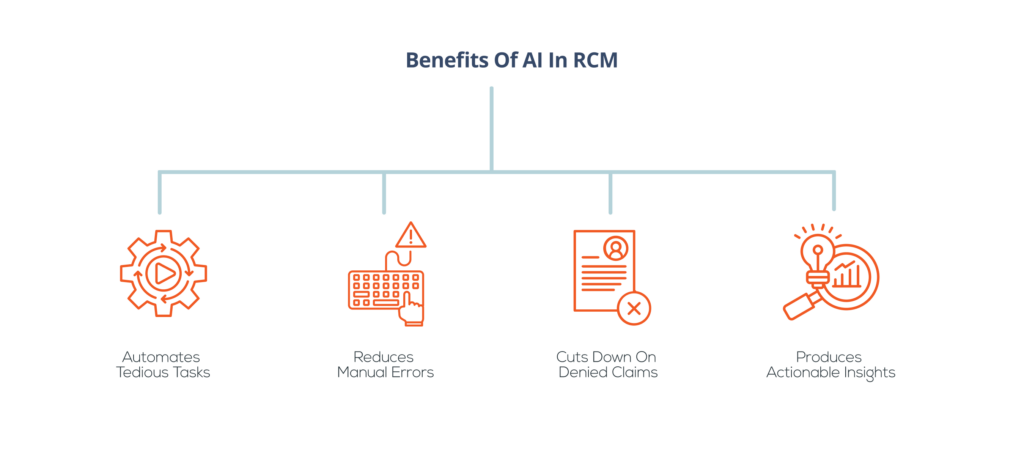
AI tools are perfect for repetitive tasks like coding, data validation, and other types of data entry.
Incorporating AI can allow staff members to redirect their time and energy away from mindless tasks, like checking to see whether addresses are formatted correctly. That way, they can spend more time and energy on work that is more strategic or empathetic—which is also much more fulfilling.
Because data entry tasks are ripe for human error, using AI can have outsized benefits here. These tools can help streamline your data entry process, shorten your revenue cycle, and increase your team’s productivity.
Just remember that AI also makes mistakes—sometimes big ones that can have serious repercussions for patients, like claim denials or inaccuracies in a treatment plan—so it’s imperative to also have rigorous staff-conducted quality assurance and audit protocols in place.
Reduce Insurance Denials
Insurance denials continue to pose problems for healthcare organizations and patients. Multiple media investigations have found that insurers are denying claims at a higher rate today than in previous years; according to PBS, one insurer was denying claims at rates exceeding 80 percent in 2020.
Some of these denials are unavoidable, especially because insurers have also been exposed as using AI to automatically deny claims within seconds.
For those that are preventable, however, AI “claims scrubbing” tools can be effective. One of the top three reasons for claims being denied is missing or inaccurate data. These scrubbing tools can go through thousands of claims at a time, flagging inaccuracies in coding, missing or inaccurate information, and other problems that could lead to a claim being denied.
Provide Actionable Insights into Trouble Areas with Analytics
AI-powered analytics are a powerful tool for any RCM team, as these programs can help identify which procedures, processes, payers, or even times of year are impacting your revenue cycle in a multitude of ways.
There are four types of analytics that RCM teams can benefit from, all of which incorporate some form of AI:
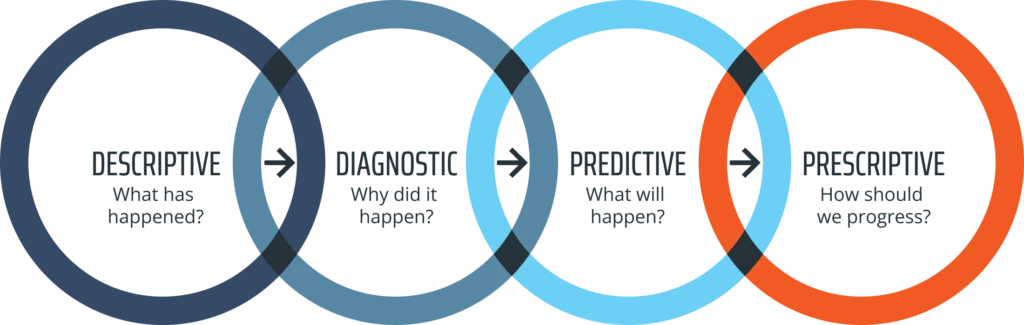
- Descriptive analytics, which draws conclusions from past data, can help you identify areas for improvement and learn from past successes and failures.
- Diagnostic analytics, which look more deeply into the root causes of RCM issues, can provide you with insights into the hidden reasons for specific changes or problems, like an increase in claim rejections within a certain period of time.
- Predictive analytics, which predict future trends based on past data, can help you strategically plan for the future and identify areas for improvement.
- Prescriptive analytics, which offer a blueprint for the best course of action going forward, can give you actionable ways to apply what you’ve learned toward the best possible outcome, both for your bottom line and your patient experience.
Whether you’re using all four types or just one, you know how valuable these tools can be. Without some form of analytics, it’s difficult to know how to improve, or even how well your RCM team is accomplishing its goals. With a strong foundation of data analytics, your team can hash out the best path forward, drawing from their years of RCM expertise to filter and refine the AI-driven recommendations.
Potential Problems with Implementing AI
Now that we’ve covered some of the most effective applications of AI, let’s take a look at the other side: the potential concerns and pitfalls that your team should be aware of.
Decrease in quality of customer service interactions
If you’re considering implementing a customer-facing AI chatbot, it’s critical to ensure that the tool is improving your patient interactions—or at least, maintaining your current level of service.
Here’s a great example. Let’s say your staff is stretched thin and unable to spend the ideal amount of time with each patient. They’re getting bogged down in answering simple questions, explaining bills, and correcting patient information. As a result, team members have less time to spend with each patient, and because they are also overworked, the quality of their patient interactions is suffering.
In this case, implementing a chatbot that can answer these types of simple billing questions, correct patient information upon request, and do other easy, data-oriented tasks could provide a great improvement in your customer interactions. Staff are freed up to focus on more complex patient needs, and patients are able to quickly get answers to questions without waiting on hold or waiting for an email reply.
If, however, a chatbot is implemented as a replacement—if patients have to struggle to get in touch with a human agent because all requests are funneled through the AI—that’s more than likely going to result in worse customer experiences (and reduced cash flow in turn).
Potential for Ethical Issues and Privacy Concerns
Another huge issue to consider when implementing any AI tool is the potential for privacy or ethical problems.
AI programs have been found to have implicit biases, which can have serious consequences for patients. Let’s consider AI programs that predict how likely a patient is to pay their bill.
If the program is running on biased data, it could produce skewed propensity to pay scores based on criteria like gender, race, or even address. This can help perpetuate discrepancies in willingness to seek care and in the quality of care sought or received.
When it comes to privacy, all AI tools used in the healthcare space must comply with HIPAA regulations. Any AI tool you consider should state clearly that it is suitable for the healthcare industry. Regardless, every AI program or tool should be seriously and properly vetted before you decide to adopt it.
How Your RCM Team Can Get Started with AI
Once you’ve decided to explore AI as an option for your team, how do you get started? Here’s a step-by-step process.
Identify the ideal use case for your organization.
Start with just one area where you want to investigate the potential for AI implementation. That could be customer service, staff training, data validation, billing, or another area. Narrowing down your options will allow you to spend enough time figuring out what’s right for your particular need without getting distracted by the hundreds of shiny new AI tools on the market.
Choose a tool that will show value quickly.
In most cases, and especially if your organization is new to AI, it will make sense to choose a tool that will create value right away. This will make it easier to achieve staff and leadership buy-in, opening up the possibility for further investments in AI down the line.
On the other hand, if your leadership and staff are already open to the possibilities of AI, you may have more latitude in choosing something that will require more of a long-term investment. No one knows your organization like you do, so exercise your judgment on what type of AI will go over the best with your team.
Invest in training for staff.
No tool, whether AI-based or not, will deliver value if staff don’t know how to use it effectively. Make sure you prioritize training on whatever AI program you choose and offer ongoing training as needed. Staff should feel empowered to ask questions when they don’t understand something, and have opportunities to explore various uses of the new tool so each team member can get the most possible value from it.
Once the tool is implemented, gather feedback from both your staff and your customers to determine how well it’s working. Remember, even as you incorporate artificial intelligence into your workflows, it’s still that irreplaceable human perspective that will help you understand where AI is falling short, how it can be improved, and what areas are better off without the influence of AI at all.
How Else Can AI Shorten Your Revenue Cycle?
Today’s healthcare organizations are operating in a challenging landscape. From staff shortages to increased reliance on patient payments, the problems facing revenue management teams are many—but AI, when properly implemented and carefully balanced with human expertise, can help you overcome them.
To learn more about how artificial intelligence and high-quality data can help propel you toward unprecedented financial success, start with our latest piece on RCM data quality, “The Role of Data Quality in the Revenue Cycle.”
Or if you’re ready to enhance your RCM performance right away, explore our debt collection services today. We strive to maintain the perfect balance between human and artificial intelligence in our collection strategies, leveraging technology to improve ROI while preserving that much-needed human touch.


