When RCM staff have the support they need—strong training, opportunities to advance their expertise, and a culture that celebrates ongoing learning and growth—they can become a key force in preventing denied claims.

Handling denied claims costs healthcare providers nearly $20 billion a year, and that number is only going up. But here’s the good news: Almost 90% of denials are preventable, and many of them are due to simple human error. With the right training and culture of support, those manual errors can be sharply reduced, and perhaps even eliminated.
Common Causes of Claim Denials
While there are hundreds of reasons claims can be denied (and even more denial codes to communicate those reasons), most denials boil down to one of these primary causes:
- Missing or incorrect information. A patient’s name could be misspelled, or the diagnosis code left blank.
- Non-covered services. A patient’s plan may not cover certain services or procedures, even if the patient’s coverage is current.
- Bundled services. Many preventive and standard services are bundled together under one umbrella code, even if each service also has its own code. Pulse oximetry is one example—if a patient comes into your office for a procedure, no matter what it is, chances are they will have an electric pulse oximeter placed on their finger to monitor their oxygen. Because this is part of a routine visit, the payer will probably bundle it under a code for evaluative services. If your office also submits a claim specifically for pulse oximetry, that claim will be denied.
- Medical necessity. Payers sometimes deny claims by saying that a procedure was not medically necessary—even though the medical professionals recommending it clearly believed that it was. This is a complex category because many payers, most notably Cigna, have been discovered to be automatically denying claims due to lack of necessity without actually reviewing the claims.
- Duplicate claims. If a claim is submitted more than once, it can automatically be denied.
- Patient eligibility. If a patient’s eligibility for a service has expired, the claim will be denied.
- Timely filing. If a claim isn’t filed within the payer’s prescribed timeframe, it can be automatically denied.
Creating a Culture of Denials Reduction
Creating a culture of denials reduction isn’t that different from creating a culture that values continuous learning, growth, and progress—the former can’t exist without the latter.
At Revco, we’ve integrated some high-level ideas to shape our culture and empower our staff.
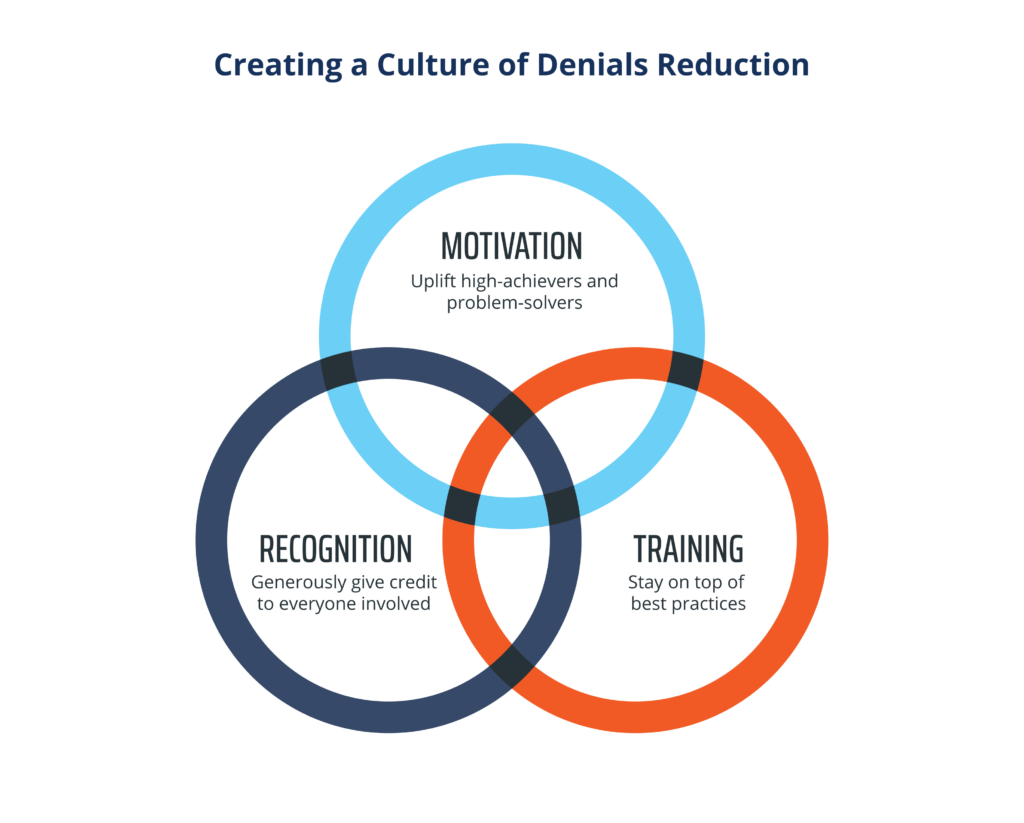
- Motivation
Motivating your staff should be done through uplift and support, rather than through overly critical or punitive measures.
While it’s always important to encourage staff toward a goal of fewer denials, in our experience, having a “zero tolerance” mindset can be counterproductive. You can easily end up with staff who feel unable to achieve a goal of zero preventable denials, and therefore unmotivated to put in their best work. We’ve always found it to be more incentivizing to reward our staff members who have low to no preventable denials than to punish those who do not.
At Revco, we’ve learned that the most effective motivation is the kind that uplifts our high-achieving staff, recognizes staff who resolve difficult cases, and contributes to a culture in which everyone feels that they are working toward a common goal. - Recognition
Everyone who worked to resolve a difficult denial deserves recognition, not only the representative who worked the phones. There’s also administrative staff who conducted research, gathered information, and located the necessary filings. We work hard to ensure that the work of these back office staff members doesn’t go unnoticed, giving credit generously to everyone involved. - Investment in comprehensive, ongoing training
Payer policies change, and this can be especially true when it comes to denials. The only way to keep your staff performing their best is to ensure your organization is staying up to date with payers’ current policies. This is best done by keeping ongoing, open communication with payers, and by implementing denials management analytics that can uncover patterns in denials over time, so that any changes can be identified early.
performance-driving RCM insights?
Targeted Steps to Reduce Denials
There are several points along the revenue cycle at which denials can occur. Here, we’ll go through the primary ones and offer a few actionable training steps that will help reduce your denials.
Patient Access
Denials in this category are due to:
- Failure to obtain pre-authorization or certification
- Non-covered services
- Inaccurate patient or insurance information gathered at registration
To address these issues, staff need to be trained in efficient and accurate patient registration practices. This means verifying demographic data and verifying insurance coverage, including informing patients about any non-covered services before they are performed.
Staff should also be trained to recognize complete vs. incomplete orders so that they do not submit anything that could likely end in a denial.
In non-emergent situations, staff should remember that taking time to perform thorough insurance checks and gather all necessary information is preferable to rushing—time may be saved upfront, but it will result in much more frustration for the patient and healthcare staff after the fact if the claim results in a denial.
Case Management
Case management-related denials can be due to:
- Lack of documentation to support level of care or length of stay
- Documentation that is not provided in a timely manner
- Documentation that does not adequately support medical necessity
To manage these types of denials, staff need to be aware of payers’ timelines and deadlines, and be empowered to obtain this information from the medical and care staff if it is not available in a timely manner.
If a staff member can identify that certain documentation is lacking—for instance, to support the length of stay—they can then communicate with the physician or care staff to get additional documentation, reducing the chances of a claim denial.
Health Information Management
This area is one of the top culprits for manual errors. An automatic denial can result from:
- A typo in a patient’s name or address
- Inputting a secondary payer as a primary payer
- Coding errors
- Any other errors in information collection regarding a patient and their care
While training is certainly key in terms of educating staff on the importance of accuracy, this area is one that can greatly benefit from an automated system that reviews and checks patient data.
Medical coding quality should be validated by an outside organization if possible, but if not, regular internal audits can go a long way toward the goal of zero preventable denials.
Information Systems
Denials that occur due to information systems issues can be caused by:
- Lack of analytics that show patterns in denials
- Difficult or non-intuitive user interfaces
- Lack of training on new systems or lack of ongoing training for current systems
To prevent these types of denials, staff should receive ongoing training on the systems they’re expected to use to gather patient data, submit claims, and analyze results.
If your system is outdated or clunky, investing in a better one should be a top priority. While it will require a large expense and effort initially, the long-term boost in efficiency, along with cost and time savings, will be much greater.
Benefits of Staff Empowerment in Denials Management
When all staff are empowered with the training, knowledge, and support they need to reduce denials, the benefits go beyond your bottom line (although that will benefit greatly, too!).
Shared sense of purpose
When reducing denials is established as an organizational goal and staff have what they need to accomplish that goal, your team will have a sense of shared purpose. This type of environment is much more conducive to the kind of collaborative teamwork that is required to effectively reduce denials and meet other organizational goals.
Better documentation organization-wide
When staff know that everyone has a part to play in reducing denials, it sets a standard for more accurate, thorough, and complete documentation by everyone from physicians and care staff to back-office administrators.
Greater efficiency
A reduction in denials can translate to greater efficiency throughout other areas of RCM, as less time must be spent tracking down codes and filing appeals and more resources can be invested in the tech and people that will help your entire RCM team flourish.
Healthier cash flow
The more denials your team has to take action on, the more delayed payments your organization must deal with. A reduction in preventable denials will boost your cash flow, leading to greater long-term financial health.
More engaged and fulfilled staff
Staff who are encouraged and able to meet their organizational goals are happier, more satisfied, and have better mental health than those who work in organizations where goals and values are not aligned.
With the post-pandemic staffing shortages and turnover rates that are still plaguing the healthcare industry at large, taking steps to invest in staff morale is more important than ever.
How to Get Started
As any experienced leader knows, change takes time—especially when it’s change across departments or an entire organization.
By setting goals early and often, and implementing incremental changes, you can transform your RCM team’s approach to denials management. Here are just a few things to keep in mind.
- Don’t wait until you have lots of material to hold a training session. Instead, conduct smaller, targeted sessions more often. This will make it easier for team members to integrate what they learn into their work right away.
- Don’t be afraid to host as-needed training sessions. If something comes up that needs to be addressed with your team, do so. This is how you begin to create an environment of continuous learning.
- Implement cross-training if possible. Staff who are cross-trained are not only more adaptable but also better at collaborating and seeing the “big picture.” Cross-training can also help staff see how important their particular role is to a larger process or goal.
- Make communication a top priority. Change has to start from the top, and your team leaders need to continuously communicate the importance of denials management and how they plan to support staff members in meeting team goals.
A final step your organization can take to cut down on denials and win more appeals is partnering with a team that specializes in denials management. We’ve built our business on a healthy, performance-driven team culture, and we can overturn denials at any stage: early, late, or even closed.
If you’d like a partner that will free up your cash flow and help you proactively prevent denials, connect with our team today.
Thank you for joining us!


