From embracing patient-centric operations to managing labor shortages and reduced cash recoveries, RCM leaders have a lot on their plates this year. Staying on top of these trends will require effective partnerships, creativity, and a forward-thinking organizational mindset.

Effective and efficient revenue cycle management is key to providing quality care to patients—and never more so than today.
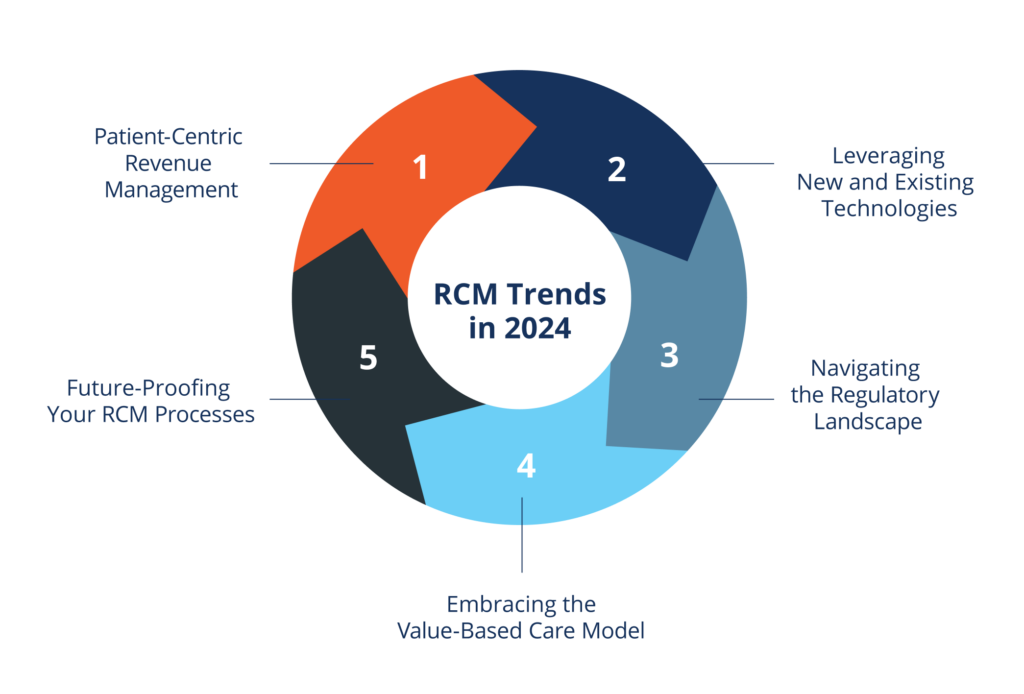
According to the latest available data, more than half of hospitals were not profitable in 2022. Becker’s Hospital CFO Report found that profitability in 2023 was inching upward, but it’s still below pre-pandemic levels. RCM leaders and healthcare CFOs are tasked with helping to reverse this troubling trend and reestablish (and eventually surpass) pre-pandemic levels of performance. This year, that will involve aligning your organization with five key trends:
- Shifting toward patient-centric revenue management
- Integrating and leveraging both new and existing technologies
- Navigating the regulatory landscape
- Embracing the value-based care model and its effects on RCM
- Future-proofing your RCM by addressing the ongoing labor shortages and declining cash recoveries
Doing so requires strong collaboration, both internally across departments and externally with partners that can support your financial success.
Let’s take a closer look at what this means.
The Shift Towards Patient-Centric Revenue Management
One of the most important trends this year is the continued shift toward patient-centric revenue management. It’s no longer a nice-to-have, but an absolute must.
Two critical factors underpin this reality:
First, patients are now the fastest-growing source of payment for healthcare organizations, rather than insurers.
Second, patients have the same expectations for paying their healthcare bills that they do for their credit card or utility bills—they want easy, convenient, and flexible options that they can complete via mobile devices.
Enhancing Patient Engagement and Transparency
Patient engagement—involving the patient in their own healthcare decisions—is frequently cited as an important clinical element of the value-based care model.
However, patient engagement throughout the revenue cycle is just as important, especially because the patient experience doesn’t end when they leave your office, are discharged from the hospital, or log off their telehealth visit.
Every interaction they have with your brand throughout the payment process, whether that’s your online billpay portal or a recovery representative, is part of your patient engagement. And better patient engagement translates to improved patient experience.
Actions you can take to improve patient engagement include:
- Opting for simplified, comprehensible billing statements
- Training RCM staff to explain patients’ charges in clear and compassionate terms, or employing partners who do so
- Communicating with patients via their preferred method (text, email, paper, etc.)
Implementing Advanced Patient-Centric Payment Solutions
Without a revenue cycle management system that prioritizes patient experience, your organization is operating at a significant disadvantage—and recent data provides clear evidence of this.
According to the Healthcare Financial Management Association, more than 50 percent of patients expect more online interaction with their healthcare providers, and one-third of all patient payments are made online. RCM strategies going forward should include patient-centric payment options like:
- Mobile pay options
- Allowing patients to keep a credit card securely on file
- Flexible payment plans that are offered proactively
- An easy-to-navigate online patient portal where payments can be made
performance-driving RCM insights?
Integrating Cutting-Edge Technologies in RCM
Today, healthcare organizations have more data available than they’re able to effectively put to use. But data analytics programs that analyze past trends, as well as predictive analytics programs, can bring some order to the chaos and yield powerful insights.
Leveraging Big Data for Informed Decision Making
“Big data” refers to the truly massive amounts of data that are generated daily by internet users, be they individuals, corporations, or other organizations.
Left on its own, big data offers little in the way of enlightenment. Advanced data analytics programs are required to make sense of the hundreds or thousands of data points a healthcare organization could generate in a given amount of time.
With the help of these programs, healthcare revenue cycle teams can identify opportunities for improvement as well as areas that need immediate attention.
Advanced programs for debt collection analytics and denials management analytics can be used to:
- Discover the optimal time of day to send email correspondence, based on patient open rates at different times
- Determine which patients are less likely to pay their bill based on past behavior, so staff can plan to devote more time to their cases or divert their energy to patients with a higher propensity to pay
- Identify patients who may need financial assistance, allowing RCM staff to offer personalized payment plans or connect them to financial assistance programs
- Understand why certain payers are denying more of your claims—and take the right steps to remedy the problem
The Impact of Automation and AI on Efficiency
The AMA found that inefficiencies during the RCM process can result in a revenue loss of between five to ten percent for healthcare organizations— a massive reduction in revenue.
Automation and AI can bring drastic improvements to healthcare organizations, especially in repetitive and burdensome areas like billing and coding. The improved accuracy that these tools offer can also help minimize claim denials.
AI is at work in any predictive analytics system your organization may use, as the program is looking at past data in order to formulate predictions about future behavior or needs.
Another development RCM leaders should be aware of is robotic process automation (RPA). This technology uses software robots to automate tasks like payment posting and data entry across different systems.
By enlisting AI and automation programs to take some of the administrative burden off of staff, healthcare organizations can boost their efficiency and redirect staff time toward tasks that require human compassion and creativity.
One important note: Any AI or RPA tool must be vetted carefully before being adopted, especially given patient privacy concerns and HIPAA regulations. The technology is advancing, but still far from perfect.
Navigating the Changing Landscape of Healthcare Regulations
With recent regulatory changes creating evolving compliance standards, healthcare revenue cycle management staff must be ever more agile and attuned to changes that affect operations.
Understanding and Adapting to New Policies
The No Surprises Act, which mandates greater pricing transparency from healthcare providers, is a definite improvement for patients.
However, this and other recent regulatory changes around things like telehealth and patient privacy means RCM staff are often left scrambling to fill greater compliance requirements without having the time to truly understand the new policies or prepare to adapt to them.
What this requires from RCM teams is a commitment to agility and a willingness to be flexible from day to day. This, in turn, requires organizations to do the difficult but imperative work of investing in keeping their team members satisfied and fulfilled on the job.
With an industry-wide labor shortage already causing problems for revenue departments, hiring new staff to assist is often not an option. In these cases, partnering with an outside RCM company can be a smart investment
The Role of Cybersecurity and Data Protection
The importance of cybersecurity and patient data protection cannot be overstated.
In 2024, healthcare organizations that do not employ the industry standard or better in cybersecurity measures risk serious data breaches and all the negative outcomes that could mean for their reputation.
They also risk leaving money on the table, as patients want to be able to store their credit card information, automate payments, and employ other online payment methods that require that their data be safe and protected.
Embracing Value-Based Care and Its Implications for RCM
The traditional fee-for-service model, which pays providers based on how many patients they see and how many services they provide, is increasingly being replaced by a focus on delivering value and quality outcomes for patients—the value-based care model.
This shift is being driven not only by regulatory changes, but also by the recognition that patient-centric care is vital for both improved health outcomes and financial sustainability.
As healthcare providers continue to move toward value-based care principles, RCM processes must accommodate these changes.
Prioritizing Quality Metrics and Patient Outcomes
Since value-based care puts quality and patient outcomes at the center, RCM teams must do the same. To that end, metrics that measure service quality and patient experiences, not just financial outcomes, should be incorporated into any RCM team’s KPIs. At the very least, RCM teams should be attuned to how these metrics are impacting their financial performance and their ability to create a stellar financial experience for patients.
Examples of quality metrics include:
- Patient access rate, or how easily a patient can access the care they need
- First-pass resolution rate, or the percentage of patient inquiries that are resolved within the patient’s first contact
- Patient satisfaction score, which should include the billing process as well as quality of care and communication
Future-Proofing Your Practice: Proactive Strategies in RCM
RCM leaders will have to overcome two major challenges facing the healthcare industry in 2024: the industry labor shortage and reduced cash recoveries resulting from that shortage.
The RCM Labor Shortage
While the labor shortage among frontline medical staff like nurses and physicians has gained great attention—rightfully so—medical administration has also been affected.
In 2022, nearly half of revenue cycle leaders said their departments were facing severe labor shortages. Today, the same challenges persist: According to a 2024 article from Becker’s, hospital CEOs ranked workforce challenges (including personnel shortages, staff burnout, and other workforce issues) as their most pressing concern in 2023.
This is exacerbating other challenges facing RCM departments, like increased complexity in billing caused by regulatory changes and changes within the payer system. And when departments are short-staffed, the workload on other team members is greater, which can contribute to further burnout among current employees.
Of course, in addition to staffing problems, labor shortages can also have a serious impact on your RCM department’s efficiency and your organization’s overall financial success. This can result in declining cash recoveries, longer revenue cycles, and decreased cash flow.
A few strategies RCM departments and healthcare organizations can employ to counter the labor shortage include:
- Outsourcing RCM and collections to a dedicated partner
- Investing in employee appreciation and culture improvement programs
- Utilizing AI and other tools to reduce the amount of repetitive, “mindless” work staff must complete
Grow Stronger Financially with Revco’s Cutting-Edge RCM Services
At Revco, we’re driven by excellence.
Our winning combination is an analytics-driven approach that’s paired with a recovery team trained to treat your patients with the utmost dignity and respect. We’ve been doing patient-centric RCM since before the term was popularized, and we’re committed to staying two steps ahead of the curve.
If you’re ready to reach a new level of financial sustainability, reach out for a consultation about our early out, debt collection, and denials management services.



